What is prostate cancer? A Necessary Summary
The prostate gland is a tiny, walnut-shaped reproductive gland that is located below the bladder and in front of the rectum in men. Prostate cancer starts there. The major job of this organ is to make a fluid that feeds and moves sperm during ejaculation.
Learning About Prostate Cancer: How It Grows
Prostate cancer happens when the DNA in prostate cells changes, which makes these cells grow too quickly. When they come together, they become lumps or tumors that can stay in the prostate for years. But in more serious cases, cancer cells can invade adjacent tissues or move through the blood and lymphatic systems to reach organs like bones or lymph nodes.
Why Prostate Cancer Is Important in 2025
There will be roughly 313,780 new instances of prostate cancer and 35,770 fatalities from it in the U.S. in 2025. That means that almost one person is diagnosed with prostate cancer every two minutes, and one person dies from it every 15 minutes. When prostate cancer is localized (just in the gland), the five-year survival rate is over 99%. But when it spreads, the survival rate lowers to about 32–40%. So, finding the problem early is crucial for changing treatment and getting better results.
Table of Contents
Fact 1: Prostate cancer is very common.
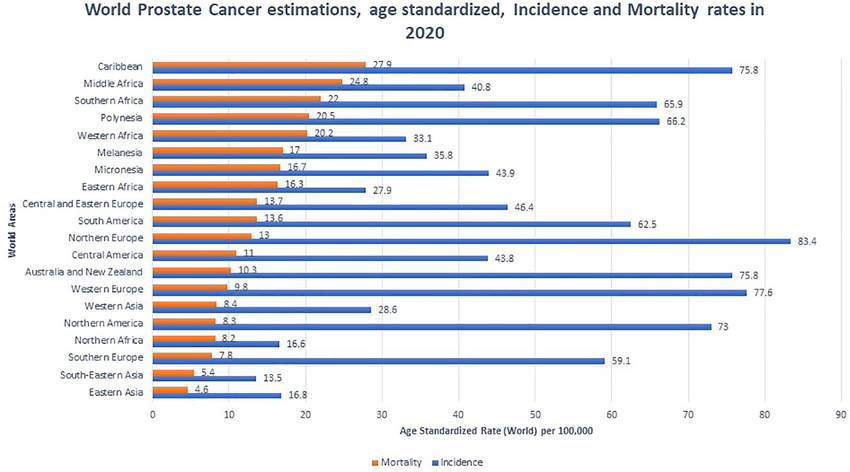
Prostate-cancer is one of the most common malignancies that men get. The American Cancer Society thinks that in 2025, there will be about 313,780 new cases and 35,770 deaths in the U.S. alone. This estimate means that prostate cancer will be responsible for an astonishing 15% of all new male cancer cases this year. It is the second most frequent cancer in men in the world, with more than 1.4 million new cases in 2022.
The Risk of Prostate-Cancer Over a Lifetime
About 60% of cases are found in men 65 and older, and the average age for diagnosis is around 67 years. The number of new cases keeps going up as life expectancy around the world, especially in industrialized countries, increases.
Why It Matters to Know How Common It Is
The fact that prostate cancer is so common shows how important public health efforts are:
- It creates screening rules and campaigns to raise awareness.
- Understanding the commonality of prostate-cancer encourages men to confidently discuss their prostate health with doctors, particularly if they are 50 years old or older or 45 years old or older if they are at higher risk.
- Localized cancer has very high survival rates, and early diagnosis leads to improved treatment outcomes.
Fact 2: The number of people getting prostate-cancer has been going up since 2014.
The Reason Prostate-Cancer Rates Went Up Again
Prostate-cancer rates started to rise again after a drop between 2007 and 2014 when PSA screening rates went down. From 2014 to 2019, the number of new diagnoses went up by about 3% each year. More recent data until 2021 show that the tendency is still quite strong: localized cases rose by around 2.4% each year, and diagnoses at later stages surged by almost 4.8% per year.
What It Means for Men's Health
- A growth in the number of prostate-cancer diagnoses, especially late-stage ones, means that we need to find better ways to catch the disease early.
- Men should work with their healthcare providers to make informed, tailored decisions about screening.
- A renewed focus on evidence-based PSA testing, along with improved imaging (mp-MRI, PSMA PET), will help find malignancies early and lower the death rate.
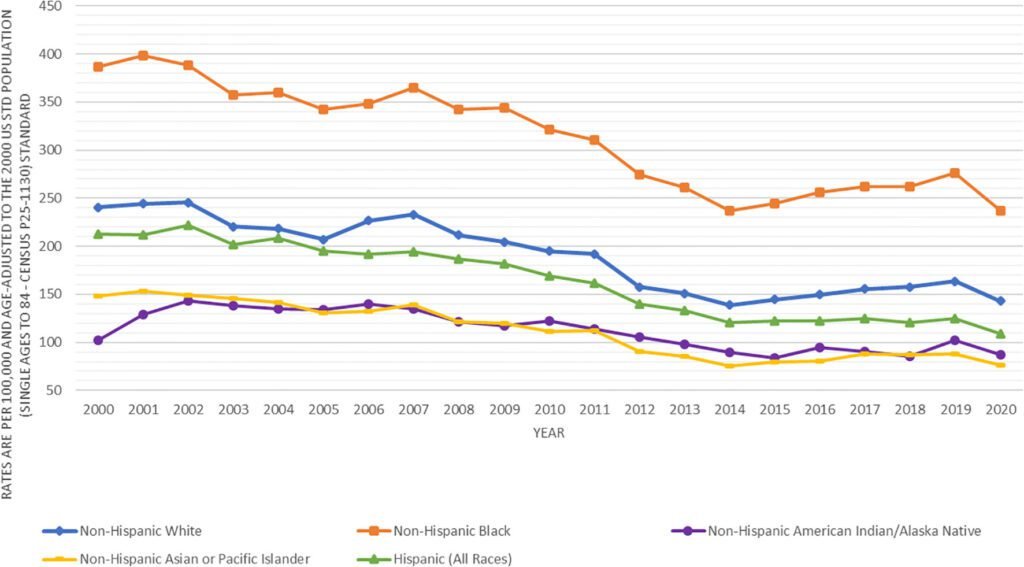
Fact 3: There are big differences in the risk and outcomes of prostate-cancer.
Groups at High Risk for Prostate-Cancer
Not all men have the same chance of getting prostate cancer. Black men and people with a family history of genetic abnormalities are two populations that have far greater incidences of the disease, more severe cases, and worse outcomes.
1. Disparity Among Black Men
According to data from 2025, prostate cancer is the most common cancer in Black males, accounting for over 44% of all invasive malignancies in this group. Black men are 1.7 times more likely than White men to get prostate cancer and 2.1 times more likely to die from it.
2. Family and genetic risk
Having a family history of prostate or breast cancer greatly raises the risk. Men who have BRCA1 or BRCA2 mutations are far more likely to get the cancer, and BRCA2 carriers have a more aggressive course of the disease. Recent genetic studies show that inherited variables may make up as much as 60% of the risk of prostate cancer.
Fact 4: In the early stages, prostate-cancer often doesn't show any symptoms.
The Quiet Nature of Prostate-Cancer
One important thing to know about prostate cancer is that most cases in the early stages don’t display any symptoms. This sneaky nature lets tumors develop without anybody noticing, but it also makes screening tests very crucial for finding cancer early, when it is easiest to treat.
When the symptoms finally show up
- Problems with urination include trouble starting to pee, a weak stream, needing to pee a lot (particularly at night), or the feeling that your bladder isn’t empty.
- Blood in urine or semen, sometimes called hematuria or hematospermia, is common in severe disease.
- Erectile dysfunction: Having trouble attaining or keeping an erection can mean that the prostate is involved or that nerves are spreading.
Why Prostate-Cancer Screening Is Important
Because early prostate cancer doesn’t often show signs, waiting for symptoms means waiting until the disease has progressed and is tougher to treat. Therefore, proactively screening with PSA blood tests or digital rectal exams (DRE) is the best method to detect disease early.
Medical guidelines say that men who are at ordinary risk should start talking about prostate cancer screening with their partners when they turn 50. People who are more likely to get sick, such as Black men or people with a family history, should start these conversations sooner, around age 40 or 45.
Fact 5: Better prostate-cancer screening saves lives and lowers harm.
1. Promising Progress in Screening
- Micro-ultrasound (micro-US)
- It provides high-resolution imaging (around 29 MHz) that is similar to mp-MRI.
- A big worldwide trial in 2025 found that micro-US-guided biopsies found clinically relevant prostate cancer just as well as MRI-guided methods.
Another meta-analysis found that micro-ultrasound had 89% sensitivity in detecting clinically significant cancer, which is nearly equivalent to mp-MRI.
2. Imaging with AI
- New systems use AI to analyze micro-ultrasound scans. In a study from May 2025, AI-analyzed micro-ultrasound showed a 92.5% ability to correctly identify diseases and a 68% ability to correctly rule out diseases, which is better than the PSA and DRE tests (AUROC 0.87 compared to 0.75).
- This level of accuracy helps find real diseases while cutting down on unneeded biopsies.
3. PSA Thresholds That Are Unique to You
- Stanford Medicine research reveals that changing PSA levels based on a person’s genetics could greatly lower the number of false positives by customizing screening to each person’s risk level.
Fact 6: Prostate-cancer treatments have advanced significantly
A New Wave of Prostate-Cancer Treatments
Treatment for prostate-cancer is undergoing significant changes, particularly for men whose cancer has spread or progressed. New treatments, like gene-based medicines, targeted radiopharmaceuticals, and oral hormone-blocking drugs, are changing outcomes and quality of life.
Oral hormone therapies are simple to use and work well.
Relugolix, an oral GnRH antagonist, is quite popular in the U.S., Canada, and the U.K. It got the go-ahead from the FDA in December 2020 and from Health Canada in October 2023. It immediately lowers testosterone levels—96.7% of men reach castration-level levels by day 29 and stay there until week 48—without the hormonal spike that happens with older injections.A sore lower back isn’t always muscular—it may signal deeper health concern
Fact 7: Early detection of prostate-cancer greatly improves survival rates.
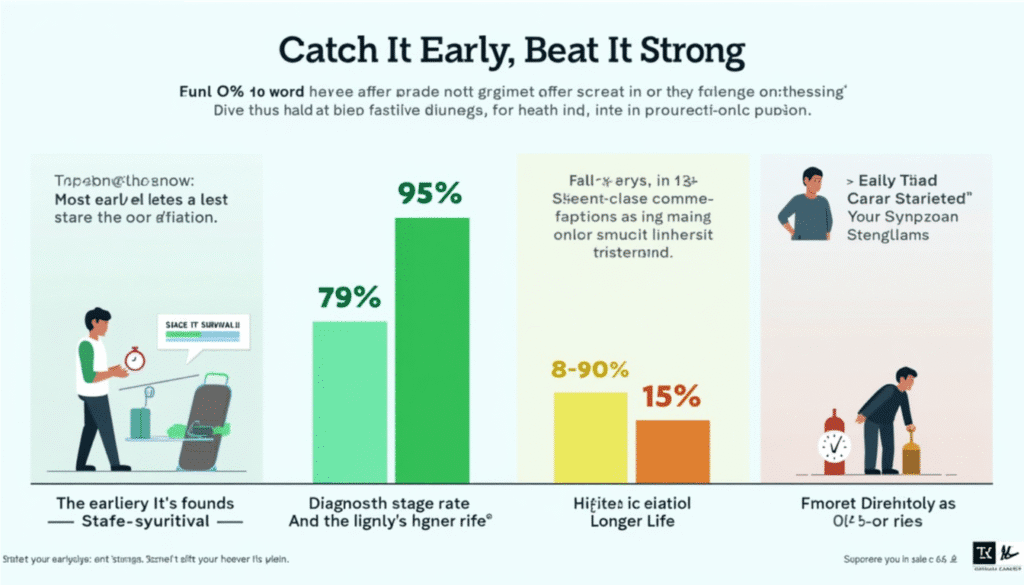
Amazing Results When Prostate-Cancer Is Found Early
One of the best things about prostate-cancer is that if it’s identified early when it’s still only in the prostate or adjacent tissues, the 5-year relative survival rate is almost 100%. Data from the SEER database (2015–2021) show that localized and regional prostate-cancers have a 100% chance of surviving for five years. Together, these two early stages account for around 83% of all cases.
When Prostate-Cancer Gets Worse
When prostate-cancer progresses from regional lymph nodes to distant organs or bones, the picture alters a lot. The SEER data suggest that the 5-year survival rate for distant-stage prostate-cancer is only about 37.9%.
More information from places like Johns Hopkins and City of Hope shows comparable numbers: the survival rate for people with distant-stage cancer is between 28% and 37%, depending on the patient’s situation and how easy it is for them to get treatment.
“If you’re experiencing lower back discomfort, check out the Top 7 Reasons for a Sore Lower Back to understand possible causes.”
Conclusion: Why will these seven important facts about prostate-cancer still be important in 2025?
You can see the problem’s size and how to improve care and prevention by knowing these 7 key facts about prostate-cancer: its prevalence, rising incidence, variability, early-stage silence, smarter screening, better treatments, and survival.
Key Points:
- There are still differences: Black males are 1.7 times more likely to be diagnosed and 2 times more likely to die, and genetic risk factors are a big part of this.
- Early prostate-cancer normally doesn’t have any symptoms; thus, screening is essential to find the disease before it becomes worse.
Better screening methods like micro-ultrasound, MRI, PSMA PET, and AI analysis are helping to cut down on unnecessary biopsies and focus on more aggressive malignancies. - Advanced prostate-cancer treatments, like oral hormone therapy and precision radiopharmaceuticals, are changing the way advanced illness is treated.
- The chances of survival are very different: for early-stage prostate-cancer, the 5-year survival probability is over 99%, whereas for metastatic disease, it reduces to about 37%.
Prostate-Cancer FAQ
1. What is prostate-cancer?
- Prostate-cancer is a disease that causes cancerous cells to form in the prostate gland, which is a small reproductive organ in men. These cells can grow slowly or quickly.
2. How often does prostate-cancer happen?
- There will be about 313,780 new cases and 35,770 deaths in the U.S. in 2025.
3. Who has a higher chance of getting prostate-cancer?
- Age (above 50, especially 65+)
- Race (Black guys are much more likely to be at risk)
- A family history of prostate cancer or genetic changes, such as those in the BRCA1/2 or ATM genes, can increase risk.
4. What are some common signs of prostate-cancer?
- Having trouble peeing, blood in urine, or semen.
- Erection or ejaculation that hurts
- Pain in the hips, back, or pelvis may occur in the later stages of prostate-cancer.